germs
‘The silence speaks the scene.’ –James Joyce

What makes some COVID patients so much sicker than others? […] Advancing age and underlying medical problems explain only part of the phenomenon […]
In an international study in Science, 10% of nearly 1,000 COVID patients who developed life-threatening pneumonia had antibodies that disable key immune system proteins called interferons. These antibodies — known as autoantibodies because they attack the body itself — were not found at all in 663 people with mild or asymptomatic COVID infections. Only four of 1,227 healthy individuals had the autoantibodies.
In a second Science study by the same team, authors found that an additional 3.5% of critically ill patients had mutations in genes that control the interferons involved in fighting viruses. Given that the body has 500 to 600 of these genes, it’s possible researchers will find more mutations.
every day, the same, again
 The eerie AI world of deepfake music — Artificial intelligence is being used to create new songs seemingly performed by Frank Sinatra and other dead stars.
The eerie AI world of deepfake music — Artificial intelligence is being used to create new songs seemingly performed by Frank Sinatra and other dead stars.
Florida man invented a robot that inserts and removes contact lenses
About 42% of 720 million Amazon reviews may be fake reviews
Duration of urination does not change with body size
Four different types of positive tears — Achievement tears are often shed in contexts of extraordinary performance or when someone overcomes an obstacle and often include feelings of pride. Beauty tears occur commonly in situations of overwhelming elegance or beauty, including nature, music or visual arts, and feature feelings of awe or experiencing chills. Affectionate tears are often experienced in situations including unexpected kindness or exceptional love such as wedding ceremonies or reunions and often feature feelings of warmth, increased communality, and feeling touched or compassionate. Finally, amusement tears are shed when something especially funny occurs and include feelings of amusement or lightness and the inclination to laugh or giggle.
How many colors are there? Quoted numbers range from ten million to a dozen. Are colors object properties? Opinions range all the way from of course they are to no, colors are just mental paint. These questions are ill-posed. […] A valid question that may replace both is how many distinguishing signs does color vision offer in the hominin Umwelt? [The umwelt theory states that the mind and the world are inseparable] The answer turns out to be about a thousand. The reason is that colors are formally not object properties but pragmatically are useful distinguishing signs.
Losing nothing is better than gaining nothing
How the White House will hand over social media accounts to President Trump [2017]
What Would We Experience If Earth Spontaneously Turned Into A Black Hole? — We’d all die. But for 21 minutes, we’d have the ride of a lifetime
China’s New Blockchain Internet
Zoom lied to users about end-to-end encryption for years, FTC says
Portland’s iconic Powell’s Books is selling a book-scented unisex fragrance
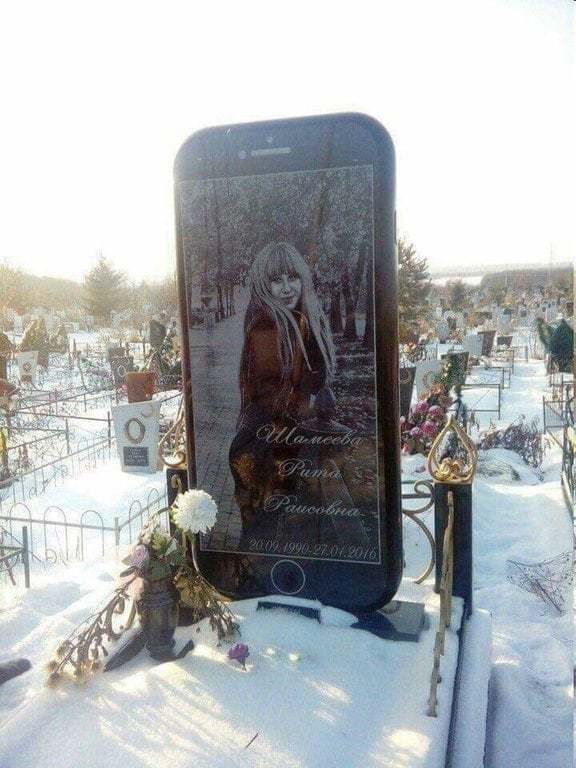
here for years
scientist and physician Eric Topol says the early results about the new COVID vaccine really are a ray of hope. He believes it might even be a so-called “superhuman vaccine… meaning it’s even more powerful than the typical human response. […] the vaccines, when we talk about 90 percent efficacy, that’s against pneumonia or getting your body infected with illness, it doesn’t sterilize the upper respiratory tract. That is the nose. And so you could be a carrier of the virus. You’re going to have to wear a mask because you won’t know if the virus is sitting” in your nose. […] We could see the virus having a hard time finding people to infect by mid-year [but] it’ll be here for years.”
As promising as the [BioNTech/Pfizer vaccine] announcement sounded, a critical question wasn’t answered: Does the vaccine prevent people from getting the infection and spreading it to others, or merely prevent symptoms? […] Another unanswered question is whether it will be possible to continue clinical trials of other vaccines. And if one later proves better than the front-runner, will it be safe to use it on people who’ve already had a vaccine with more modest benefits? What Happens to the Other Vaccines Now?
Covid Superspreader Risk Is Linked to Restaurants, Gyms, Hotels — according to a study that used mobile phone data from 98 million people
I am an imaging cardiologist who is developing diagnostic techniques to assess changes in heart muscle function in patients with COVID-19. In a study released Nov. 4, my colleagues and I found evidence of heart abnormalities in over one-third of student athletes who tested positive for COVID-19 [The Conversation]
One in 5 COVID-19 patients develop mental illness within 90 days - study
“Social distancing and mask wearing to reduce the spread of COVID-19 have also protected against many other diseases…But susceptibility to those other diseases could be increasing, resulting in large outbreaks when masking and distancing stop.”
A nasal spray that blocks the absorption of the SARS-CoV-2 virus has completely protected ferrets it was tested on, according to a small study released on Thursday by an international team of scientists. The study, which was limited to animals and has not yet been peer-reviewed, was assessed by several health experts at the request of The New York Times. If the spray, which the scientists described as nontoxic and stable, is proved to work in humans, it could provide a new way of fighting the pandemic. A daily spritz up the nose would act like a vaccine. […] The spray attacks the virus directly. It contains a lipopeptide, a cholesterol particle linked to a chain of amino acids, the building blocks of proteins. This particular lipopeptide exactly matches a stretch of amino acids in the spike protein of the virus, which the pathogen uses to attach to a human airway or lung cell. Before a virus can inject its RNA into a cell, the spike must effectively unzip, exposing two chains of amino acids, in order to fuse to the cell wall. As the spike zips back up to complete the process, the lipopeptide in the spray inserts itself, latching on to one of the spike’s amino acid chains and preventing the virus from attaching. [NY Times]
Every day, the same, again

Man shot in Russia in argument over Kant
Therapy patients blackmailed for cash after clinic data breach
researchers show that the body produces more stress hormones when people are repeatedly interrupted at work. And yet the subjects did not experience an equal rise in their consciously perceived sense of psychological stress.
People spontaneously judge others’ personality based on their facial appearance and these impressions guide many important decisions. Our findings consistently suggest that people show neither accuracy nor meta-accuracy when forming face-based personality impressions.
Commercial Features of Placebo and Therapeutic Efficacy — It is possible that the therapeutic efficacy of medications is affected by commercial features such as lower prices.
Does divorce change your personality? (the overall finding of this study suggests that experiencing a divorce is unlikely to lead to permanent personality change)
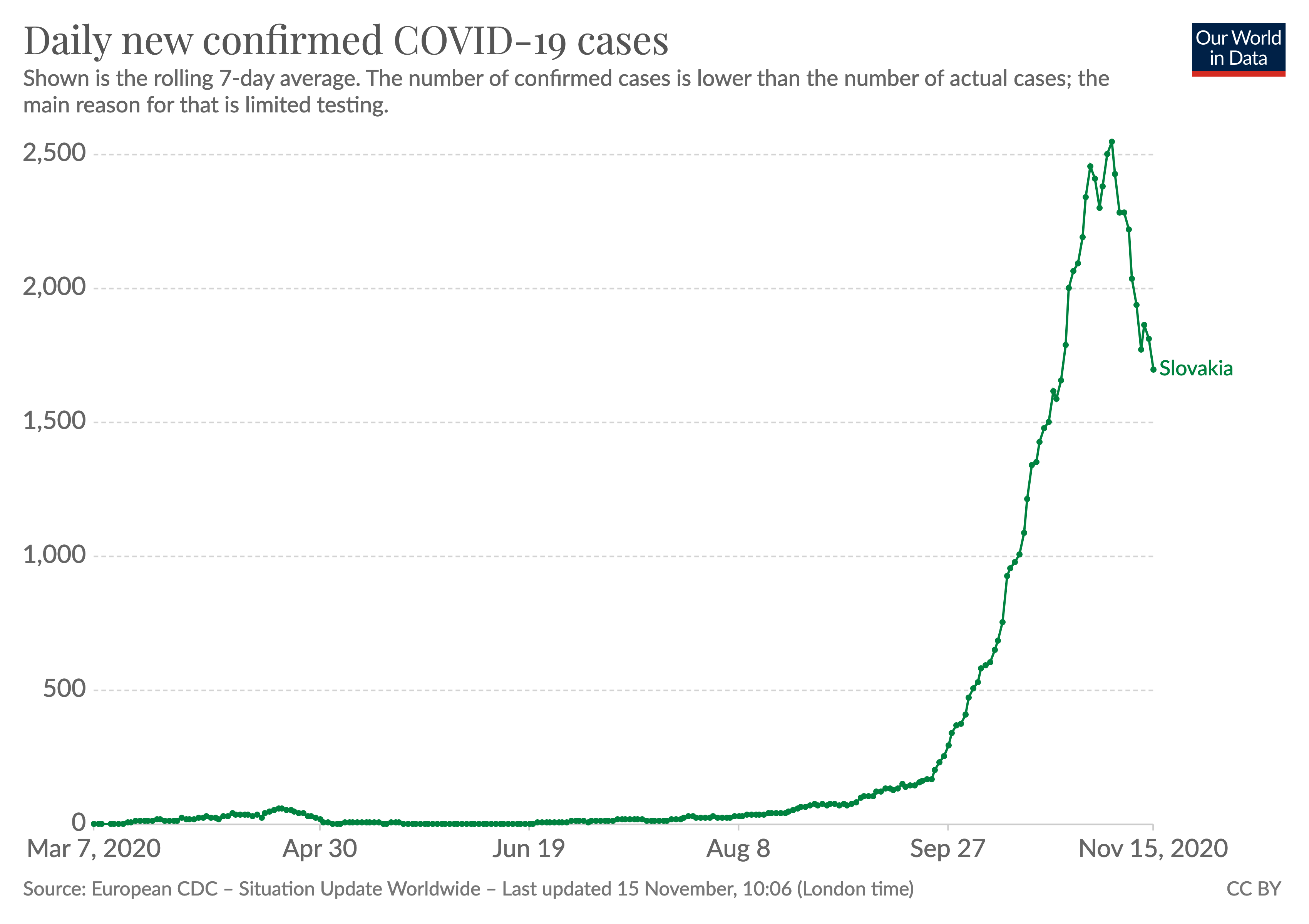
Slovakia managed to test more than 3.6 million people — two thirds of its population — in just two days […] Just over 1% of those taking part tested positive […] Those who tested negative no longer have to comply with the strictest restrictions as long as they can prove their negative status with an official certificate. People who tested positive now have to quarantine — either at home, or in one of dozens of designated hotels across the country. […] effective mass testing could be used in the long term as an alternative to lockdown to control the spread of disease.
Hong Kong will relax social-distancing measures on [Oct 30], with six people allowed to be seated at a restaurant table, up from four, while the size limit for groups in bars and pubs will rise from two to four. In a move to take effect in time for the weekend, dine-in services will also be permitted until 2am, an extension from midnight. But customers must wear a mask when not seated and are not allowed to eat or drink away from their table. [South China Morning Post]
Venice tests long-delayed flood barrier months after waters swamped city And Flood defences save Venice from second high tide More: the flood of 1966 - the water would have reached 230 cms over the average sea level.
Don’t Even Try Paying Cash in China — Most businesses there, from the fanciest hotels to roadside fruit stands, display a QR code — a type of bar code — that people scan with a smartphone camera to pay with China’s dominant digital payment apps, Alipay and WeChat. Paying by app is so much the norm that taxi drivers might curse at you for handing them cash. [NY Times]
Inside eBay’s Cockroach Cult: The Ghastly Story of a Stalking Scandal [NY Times]
Blacklight, a tool to see how the websites you visit are tracking you
These drones will plant 40,000 trees in a month. By 2028, they’ll have planted 1 billion
Is It Better to Plant Trees or Let Forests Regrow Naturally?
Why Tunnels in The US Cost Much More Than Anywhere Else in The World
This is an experiment about how we view history
The 15 weirdest works of classical music (#10 - My Lord Chamberlain is a duet for two lutenists, but just one lute.)
Silent Sleep Training Medical Didgeridoo — the solution for sleep apnea and snoring
In tomorrow’s episode
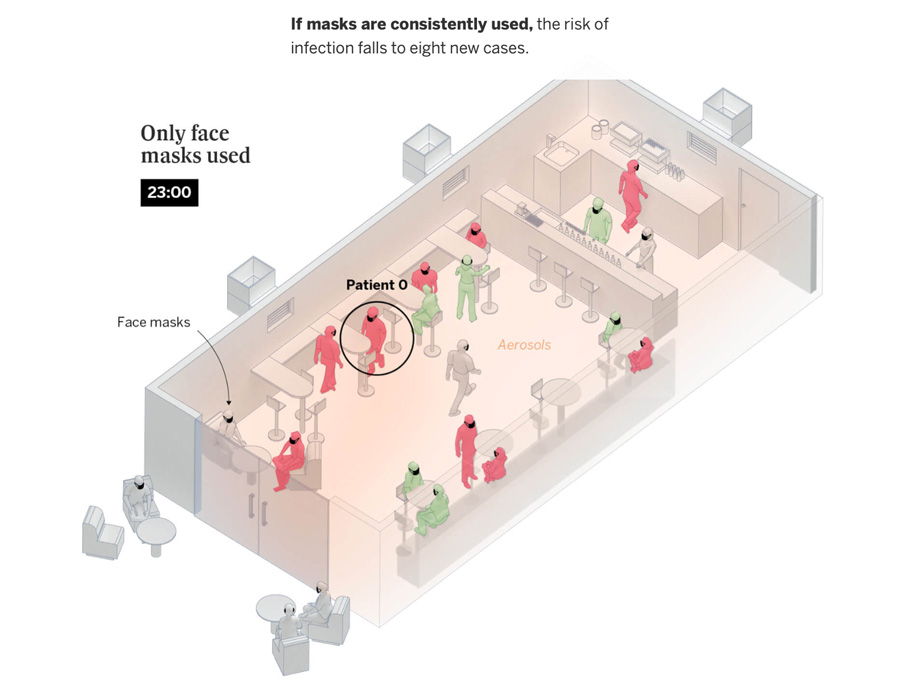
There are COVID-19 incidents in which a single person likely infected 80 percent or more of the people in the room in just a few hours. But, at other times, COVID-19 can be surprisingly much less contagious. Overdispersion and super-spreading of this virus are found in research across the globe. A growing number of studies estimate that a majority of infected people may not infect a single other person. A recent paper found that in Hong Kong, which had extensive testing and contact tracing, about 19 percent of cases were responsible for 80 percent of transmission, while 69 percent of cases did not infect another person. This finding is not rare: Multiple studies from the beginning have suggested that as few as 10 to 20 percent of infected people may be responsible for as much as 80 to 90 percent of transmission, and that many people barely transmit it.
{ The Atlantic | Continue reading | more on the k factor }
In late February, drug company Biogen held its annual conference in Boston. The United States had fewer than 20 known COVID-19 cases at the time. But one of the roughly 200 attendees must have carried the virus. It triggered a big outbreak. At least 97 people who attended the conference, or lived in a household with someone who did, tested positive. The Biogen meeting had become a superspreading event. Eventually, the virus spread from the meeting across Massachusetts and to other states. A recent study estimates it led to tens of thousands of cases in the Boston area alone. […]
A study from India published in Science last month concluded that 8% of infected people caused 60% of the secondary cases; 70% of people did not pass the virus on to anyone else.
{ Science | Continue reading }
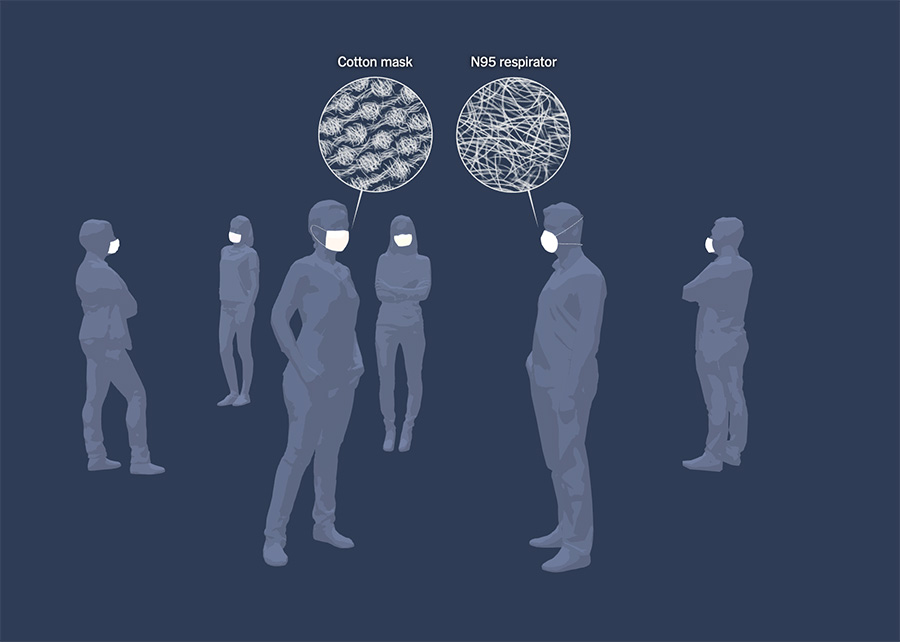
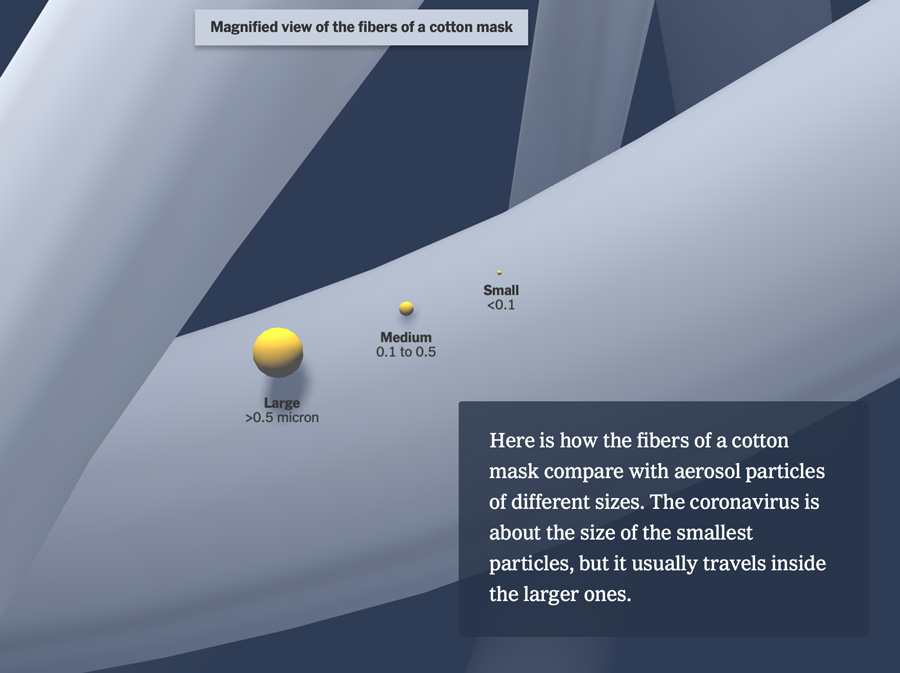
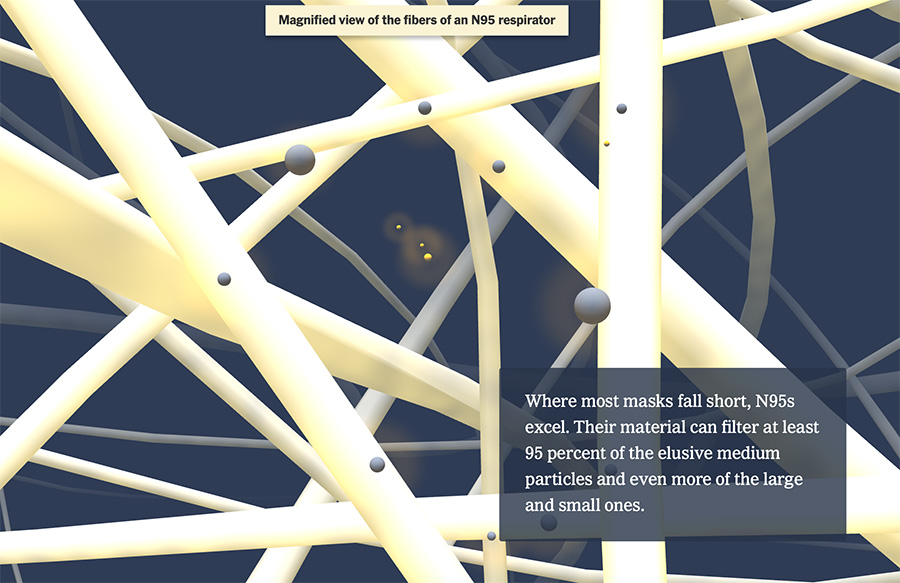
A well-fitting N95 is the gold standard, but don’t worry if you can’t get your hands on one. When everyone wears a mask, the combined filtration efficiency increases. | NY Times | full story }
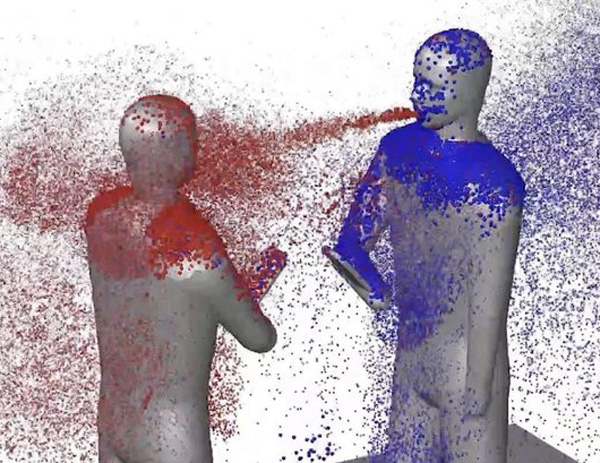
{ A room, a bar and a classroom: how the coronavirus is spread through the air | El Pais | full story }
to date, none of the vaccines being developed for the U.S. market has been proven to be effective in preventing Covid-19 disease.
and { Taiwan marks 200 days without domestic Covid-19 infection }
photo { Christopher Hainey }
Follow your plan, not your mood
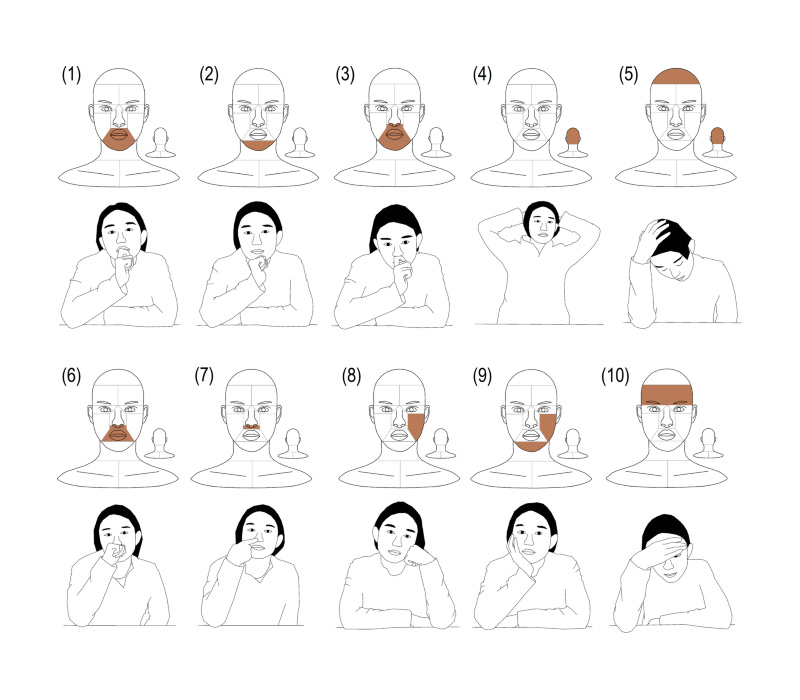
Self-touch may promote the transfer of microorganisms between body parts or surfaces to mucosa. In overt videography of a post-graduate office, students spent 9% of their time touching their own hair, face, neck, and shoulders (HFNS). These data were collected from 274,000 s of surveillance video in a Chinese graduate student office. The non-dominant hand contributed to 66.1% of HFNS-touches. Most importantly, mucous membranes were touched, on average, 34.3 (SE = 2.4) times per hour, which the non-dominant hand contributed to 240% more than the dominant hand. Gender had no significant effect on touch frequency, but a significant effect on duration per touch.
slipping out of control
 Fitness influencer who ‘thought COVID didn’t exist’ shares final message on Instagram before dying
Fitness influencer who ‘thought COVID didn’t exist’ shares final message on Instagram before dying
Achieving herd immunity without an effective vaccine would result in widespread fatalities. […] “And remember, [Michael Osterholm, a renowned infectious-disease expert, said,] when we talk about getting to 50%–70% protection, we’re talking you can get there with disease — but if that happens, there will be lots of deaths, a lot of serious illnesses — or we can try to get there with vaccination, and postponing the number of people who get sick until we have the vaccines available. 5o%–70% just slows down transmission, it doesn’t stop it. So this virus is going to keep looking for wood to burn for as long as it can … so, our goal is to get as many people protected with vaccines” [Axios]
Sudden irreversible hearing loss post COVID-19
A man caught coronavirus twice—and it was worse the second time — That makes him the fifth recorded person to have caught the coronavirus twice—and raises more questions about how immunity might work.
Slovakian Prime Minister Igor Matovic announced plans Saturday to test everyone aged 10 years and over in the country for Covid-19 […] “testing will be free-of-charge” for the population of 5.4 million. The campaign is expected to take place over two weekends starting at the end of October. It is not yet known whether participation will be mandatory. [CNN]
Coronavirus transmission is slipping out of control in Belgium, Health Minister Frank Vandenbroucke said Sunday, on the eve of new restrictions in the country. “We are really very close to a tsunami,” he warned, speaking to broadcaster RTL. “We no longer control what is happening.” New restrictions are set to take effect on Monday, including the closure of all bars and restaurants, and a midnight curfew nationwide. [Politico]
In a young, low-risk population with ongoing symptoms, almost 70% of individuals have impairment in one or more organs four months after initial symptoms of SARS-CoV-2 infection. [MedRxiv]
In two early studies, researchers said some patients showed signs of healing just weeks after leaving the hospital. […] about 80 percent of patients have mild to moderate symptoms, 15 percent develop a severe form of the disease and roughly five percent like Ms. Coissieux escalate to critical. […] Ms. Coissieux, 78, was sent to a nearby pulmonary rehabilitation clinic, Dieulefit Santé, where a physical therapist taught her breathing exercises to help restore her lungs and the muscles involved in breathing. When she went home three weeks later, Ms. Coissieux could walk close to 1,000 feet, albeit with a walker. As she continued exercising at home, she grew stronger. “Now I can walk 500 meters with no walker,” or about 1,600 feet. [NY Times]
California biotech company Vaxart, which is working on a Covid-19 vaccine, is under federal investigation and is being sued by a number of investors for allegedly exaggerating its involvement in the US government’s Operation Warp Speed program for developing Covid-19 vaccines and treatments. In June, Vaxart issued a press release that said “Vaxart’s Covid-19 Vaccine Selected for the US Government’s Operation Warp Speed.” The news helped propel Vaxart’s stock price to nearly $17, up from approximately $3, and hedge fund Armistice Capital, which partly controlled Vaxart, sold shares for a profit of more than $200 million, according to its SEC filings. A few weeks before the announcement, Vaxart granted amendments to the warrants agreements, which allowed Armistice to sell almost all of their stock, which they did once the stock price skyrocketed. In July, the US Department of Health and Human Services (HHS) told the New York Times that it had not entered into a funding agreement or negotiations with Vaxart. Vaxart has not been chosen by Operation Warp Speed to receive research funding, but instead had limited involvement, HHS told the New York Times. Vaxart’s vaccine, an oral tablet, was only involved in preliminary studies on primates sponsored by Warp Speed. [CNN]
My wife wants to make love while the President has the freaking novel coronavirus! Nice try, psycho!
Double fucked
Frederick Trump […] paternal grandfather of Donald J. Trump, […] made his fortune by operating a restaurant and a brothel in Canada […] He died from the Spanish flu in 1918.
more { Trump coughed after the word “therapeutics” and it was edited out }
related { company that sells software used in hundreds of clinical trials, including the crash effort to develop tests, treatments and a vaccine for the coronavirus, was hit by a ransomware attack | NY Times }
flattening the curve, vertically

{ COVID-19 at the White House | “He’s fucked, we’re fucked,” said one White House aide. When informed of the Biden campaign’s announcement that the former VP and his wife, Dr Jill Biden, had both tested negative, the aide replied: “Double fucked.” }
I’ve an eye on queer Behan and old Kate and the butter, trust me. She’ll do no jugglywuggly with her war souvenir postcards to help to build me murial, tippers! I’ll trip your traps!

[A]bout half of patients report neurological symptoms, including headaches, confusion and delirium, suggesting the virus may also attack the brain.
A new study offers the first clear evidence that, in some people, the coronavirus invades brain cells, hijacking them to make copies of itself. The virus also seems to suck up all of the oxygen nearby, starving neighboring cells to death.
It’s unclear how the virus gets to the brain or how often it sets off this trail of destruction. Infection of the brain is likely to be rare, but some people may be susceptible because of their genetic backgrounds, a high viral load or other reasons.
Forty percent to 60 percent of hospitalized Covid-19 patients experience neurological and psychiatric symptoms, said Dr. Robert Stevens, a neurologist at Johns Hopkins University. But the symptoms may not all stem from the virus’s invasion of brain cells. They may be the result of pervasive inflammation throughout the body.
related { ‘Carnage’ in a lab dish shows how the coronavirus may damage the heart }
O, passmore that and oxus another! Don Dom Dombdomb and his wee follyo! Was his help inshored in the Stork and Pelican against bungelars, flu and third risk parties?
The World Health Organization has said it would prefer a vaccine to be at least 70% effective, but it has set its minimum threshold for a Covid-19 vaccine at 50%. […]
According to Shearing, figures from developers suggest 1 billion doses may be available this year, with another 7 billion ready for distribution in 2021. But those numbers assume multiple vaccines are approved, and supply could turn out to be significantly lower. Specialized needles and syringes will be needed to administer the vaccine, but countries including the United States don’t have enough on hand. There’s also a global shortage of glass vials to contend with. The WHO does not expect widespread vaccinations until the middle of next year, a spokesperson said Friday.
An experimental submarine, the ‘Siren II,’ is sent to find out what happened to the missing ‘Siren I’
Researchers in Hong Kong are reporting the first confirmed case of reinfection with the coronavirus.
“An apparently young and healthy patient had a second case of Covid-19 infection which was diagnosed 4.5 months after the first episode,” University of Hong Kong researchers said Monday in a statement.
The report is of concern because it suggests that immunity to the coronavirus may last only a few months.
The 33-year-old man had only mild symptoms the first time, and no symptoms this time around. The reinfection was discovered when he returned from a trip to Spain, the researchers said, and the virus they sequenced closely matched the strain circulating in Europe in July and August.
“Our results prove that his second infection is caused by a new virus that he acquired recently rather than prolonged viral shedding,” said Dr. Kelvin Kai-Wang To, a clinical microbiologist at the University of Hong Kong.
Doctors have reported several cases of presumed reinfection in the United States and elsewhere, but none of those cases have been confirmed with rigorous testing. Recovered people are known to shed viral fragments for weeks, which can cause tests to show a positive result in the absence of live virus.
But the Hong Kong researchers sequenced the virus from both rounds of infection and found significant differences in the two sets of virus, suggesting that the patient was infected a second time.
{ NY Times | Continue reading }
Some people can get the pandemic virus twice, a study suggests. That is no reason to panic. […]
Even if the finding settles the question of whether people can be reinfected with the pandemic virus, it raises many additional questions: How often does this happen? Do people have milder infections, or no symptoms at all, the second time around? Can they still infect others? If natural infection does not always confer solid protection, will that be true for vaccines as well?
In type 1 immunity, pathogen clearance is mediated through effector cells including group 1 innate lymphocytes (ILC1), natural killer (NK) cells, cytotoxic T lymphocytes, and T helper 1 (TH1) cells

It is clear from this and other studies that the immune response in hospitalized patients with severe COVID-19 is characterized by lymphopenia and the expression of molecules associated with ongoing inflammation8, whereas these same molecules are expressed at a lower level in people with mild or moderate disease. Differences in immune responses between the different categories of disease severity are even more evident when people with very mild or subclinical disease are included in the analyses.
A key next step will be to analyse samples from people with extremely early signs of COVID-19, and to compare longitudinal data in those who do and those who don’t require hospitalization. Some people who develop severe disease seem to have a suboptimal immune response initially, which might allow uncontrolled viral replication. Such high replication might, in turn, contribute to severe disease.
related { Efforts are ongoing to find which human or viral factors underpin whether a person with COVID-19 will develop severe symptoms. Clinical evidence linked to two viral lineages now provides key insights into this enigma. | Nature }
quote { Longitudinal analyses reveal immunological misfiring in severe COVID-19 }
‘You act like mortals in all that you fear, and like immortals in all that you desire.’ –Seneca

Amid all the fighting in your airways, messenger cells grab small fragments of virus and carry these to the lymph nodes, where highly specialized white blood cells—T-cells—are waiting. The T-cells are selective and preprogrammed defenders. Each is built a little differently, and comes ready-made to attack just a few of the zillion pathogens that could possibly exist. For any new virus, you probably have a T-cell somewhere that could theoretically fight it. Your body just has to find and mobilize that cell. Picture the lymph nodes as bars full of grizzled T-cell mercenaries, each of which has just one type of target they’re prepared to fight. The messenger cell bursts in with a grainy photo, showing it to each mercenary in turn, asking: Is this your guy? When a match is found, the relevant merc arms up and clones itself into an entire battalion, which marches off to the airways.
Some T-cells are killers, which blow up the infected respiratory cells in which viruses are hiding. Others are helpers, which boost the rest of the immune system. Among their beneficiaries, these helper T-cells activate the B-cells that produce antibodies—small molecules that can neutralize viruses by gumming up the structures they use to latch on to their hosts. Roughly speaking—and this will be important later—antibodies mop up the viruses that are floating around outside our cells, while T-cells kill the ones that have already worked their way inside. T-cells do demolition; antibodies do cleanup.
Both T-cells and antibodies are part of the adaptive immune system. This branch is more precise than the innate branch, but much slower: Finding and activating the right cells can take several days. It’s also long-lasting: Unlike the innate branch of the immune system, the adaptive one has memory.
After the virus is cleared, most of the mobilized T-cell and B-cell forces stand down and die off. But a small fraction remain on retainer—veterans of the COVID-19 war of 2020, bunkered within your organs and patrolling your bloodstream. This is the third and final phase of the immune response: Keep a few of the specialists on tap. If the same virus attacks again, these “memory cells” can spring into action and launch the adaptive branch of the immune system without the usual days-long delay. […]
Many infected people still clear the virus after a few weeks of nasty symptoms. But others don’t. Maybe they initially inhaled a large dose of virus. Maybe their innate immune systems were already weakened through old age or chronic disease. In some cases, the adaptive immune system also underperforms: T-cells mobilize, but their levels recede before the virus is vanquished, “almost causing an immunosuppressed state,” Iwasaki says. […]
There are also preliminary hints that some people might have a degree of preexisting immunity against the new coronavirus. Four independent groups of scientists—based in the U.S., Germany, the Netherlands, and Singapore—have now found that 20 to 50 percent of people who were never exposed to SARS-CoV-2 nonetheless have significant numbers of T-cells that can recognize it. These “cross-reactive” cells likely emerged when their owners were infected by other, related coronaviruses, including the four mild ones that cause a third of common colds, and the many that infect other animals.
But Farber cautions that having these cross-reactive T-cells “tells you absolutely nothing about protection.” It’s intuitive to think they would be protective, but immunology is where intuition goes to die. The T-cells might do nothing. There’s an outside chance that they could predispose people to more severe disease. We can’t know for sure without recruiting lots of volunteers, checking their T-cell levels, and following them over a long period of time to see who gets infected—and how badly.
Even if the cross-reactive cells are beneficial, remember that T-cells act by blowing up infected cells. As such, they’re unlikely to stop people from getting infected in the first place, but might reduce the severity of those infections.
deterioration in the forecasts of surface meteorology
 Weather forecasts play essential parts in daily life, agriculture and industrial activities, and have great economic value. Meteorological observations on commercial aircraft help improve the forecast. However, the global lockdown during the COVID‐19 pandemic chops off 50‐75% of aircraft observations. […] We see deterioration in the forecasts of surface meteorology and atmospheric stratification, and larger deterioration in longer‐term forecasts [AGU]
Weather forecasts play essential parts in daily life, agriculture and industrial activities, and have great economic value. Meteorological observations on commercial aircraft help improve the forecast. However, the global lockdown during the COVID‐19 pandemic chops off 50‐75% of aircraft observations. […] We see deterioration in the forecasts of surface meteorology and atmospheric stratification, and larger deterioration in longer‐term forecasts [AGU]
How the Porn Industry Is Changing During COVID-19
Why the porn industry has a lot to teach us about safety in the Covid-19 era
this month, a group of prominent scientists made the case that superspreading clusters suggest the virus is sometimes being transmitted over longer distances through the air in far smaller and more numerous particles. […] Why didn’t the infamous Lake of the Ozarks party spur lots of cases, while a much smaller gathering at a Michigan bar produced nearly 200? Part of the uneven spread of the coronavirus — and the phenomenon of superspreading — can be explained by extreme individual variation in infectivity, researchers say. Overall, researchers have estimated in recent studies that some 10 to 20 percent of the infected may be responsible for 80 percent of all cases. […] One proposal, from a Moscow State University professor, calls for shifting testing resources from the general public to efforts to identify potential “super emitters” with high viral loads by using randomized testing. Other proposals focus on limiting people’s more random interactions, such as on public transit, or at bars and restaurants, while loosening restrictions on their regular contacts, such as through work or school. [Washington Post]
Professional diver Emiliano Pescarolo contracted coronavirus in March and spent 17 days in hospital in the Italian port city of Genoa before being discharged on April 10. Now, three months later, the 42-year-old still experiences breathing difficulties. “Once back home, even after weeks I couldn’t see any progress: if I took a small walk, it was like climbing Mount Everest. I was out of breath also just for talking. I was very worried,” he said. Pescarolo is one of dozens of former Covid patients now receiving care at a rehabilitation clinic in Genoa — and says he is starting to see some progress. [CNN]
Despite how unnatural social distancing may feel to people, it is very much a part of the natural world, practiced by mammals, fishes, insects and birds. Social animals stay apart, changing behaviors such as grooming to stop the spread of diseases that could kill them.